- Physician (M.D. or D.O.)
- Physician's assistant
- Nurse practitioner
- An approved Individualized Family Service Plan (IFSP) for Early Intervention PT/OT
- All Outpatient PT/OT claims must contain the valid NPI number of the OPR physician, physician assistant, nurse practitioner or provider associated with an Individualized Family Service Plan (IFSP) in accordance with Program Rule 8.125.8.A.
- The Early Intervention Service Broker may have their rendering NPI listed as the referring NPI for IFSP-ordered early intervention services. The rendering and referring must be the individual NPI for the therapist or the ordering physician.
- The new enrollment requirement for OPR providers does not include a requirement to see Medicaid members or to be listed as a Medicaid provider for patient assignments or referrals.
- Physicians or other eligible professionals who are already enrolled in Health First Colorado as participating providers and who submit claims to Health First Colorado are not required to enroll separately as OPR providers.
- Claims without a valid OPR NPI number which are paid will then be subject to recovery.
- Medical documentation must be kept on file to substantiate the order, prescription or referral for Outpatient PT/OT. Claims lacking such documentation on file will be subject to recovery.
- Early Intervention Outpatient PT/OT claims must have modifier 'TL' attached on the procedure line item for Health First Colorado to identify that the services rendered were associated with an approved IFSP.
- Any claim with modifier 'TL' attached must be for a service ordered by an approved IFSP.
- If the OPR NPI on the claim is that of the rendering provider, and the claim does not have modifier 'TL' attached, the claim is subject to recovery.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT)
8.280.4.E Other EPSDT Benefits
Other health care services may include other EPSDT benefits if the need for such services is identified. The services are a benefit when they meet the following requirements:
- All goods and services described in Section 1905(a) of the Social Security Act are a covered benefit under EPSDT when medically necessary as defined at 10 C.C.R. 2505-10, Section 8.076.1.8, regardless of whether such goods and services are covered under the Colorado Medicaid State Plan.
- For the purposes of EPSDT, medical necessity includes a good or service that will, or is reasonably expected to, assist the client to achieve or maintain maximum functional capacity in performing one or more Activities of Daily Living; and it must meet the criteria set forth at Section 8.076.1.8.b - g.
- The service provides a safe environment or situation for the child.
- The service is not for the convenience of the caregiver.
- The service is medically necessary.
- The service is not experimental or investigational and is generally accepted by the medical community for the purpose stated.
- The service is the least costly.
Payment for Covered Services
- If Prior Authorization Requests (PARs) for services are required, the following policy applies:
- Technical/lack of information (LOI) denial does not mean those services are not covered. Members may not be billed for services denied for LOI.
- Services partially approved are still considered covered services. Members may not be billed for the denied portion of the request.
- Services totally denied for not meeting medical necessity criteria are considered non-covered services.
- Members who reach the initial 48-unit limit for physical and occupational therapy (PT/OT) require a PAR to obtain further coverage. Refusal, failure or negligence by the provider to request a PAR for services beyond the first 48 units of PT/OT does not mean that those additional services are non-covered.
Medically Necessary
Outpatient physical and occupational therapy services must be medically necessary to qualify for Health First Colorado reimbursement. Medical necessity (10 CCR 2505-10 8.076.1.8) means a Medical Assistance program good or service meets all of the following criteria. The good or service:
- Will, or is reasonably expected to prevent, diagnose, cure, correct, reduce or ameliorate the pain and suffering, or the physical, mental, cognitive or developmental effects of an illness, condition, injury or disability. This may include a course of treatment that includes mere observation or no treatment at all. Is provided in accordance with generally accepted professional standards for health care in the United States.
- Is clinically appropriate in terms of type, frequency, extent, site and duration.
- Is not primarily for the economic benefit of the provider or primarily for the convenience of the member, caretaker or provider.
- Is delivered in the most appropriate setting(s) required by the member's condition.
- Is not experimental or investigational.
- Is not more costly than other equally effective treatment options.
Documentation Requirements
Rendering providers must document all evaluations, re-evaluations, services provided, member progress, attendance records and discharge plans. All documentation must be kept in the member's records along with a copy of the referral or prescribing provider's order. Documentation must support both the medical necessity of services and the need for the level of skill provided. Rendering providers must copy the member's primary care provider (PCP), prescribing provider and/or medical home on all relevant records.
All documentation must include the following:
- The member's name and date of birth.
- The date and type of service provided to the member.
- The name or names and titles of the persons providing each service including assistants and the name and title of the therapist supervising or directing the services.
Health First Colorado requires the following types of documentation as a record of services provided within an episode of care: initial evaluation, re-evaluation, visit/encounter notes and a discharge summary.
Initial Evaluation
Written documentation of the initial evaluation must include the following:
- Referral Information: Reason for referral and referral source.
- History: Must include diagnoses pertinent to the reason for referral including date of onset of relevant diagnosis, cognitive, emotional and/or physical loss necessitating referral, and the date of onset if different from the onset of the relevant diagnoses, current functional limitation or disability as a result of the above loss, and the date of onset of the disability, pre-morbid functional status, including any pre-existing loss or disabilities, review of available test results, review of previous therapies/interventions for the presenting diagnoses, and the functional changes (or lack thereof) as a result of previous therapies or interventions.
- Assessment: The assessment section must include a summary of the member's impairments, functional limitations and disabilities based on a synthesis of all data/findings gathered from the evaluation procedures. Pertinent factors which influence the treatment diagnosis and prognosis must be highlighted, and the inter-relationship between the diagnoses and disabilities for which the referral was made must be discussed.
- Plan of Care: A detailed Plan of Care must be included in the documentation of an initial evaluation. This care plan must include the following:
- Specific treatment goals for the entire episode of care which are functionally-based and objectively measured.
- Proposed interventions/treatments to be provided during the episode of care.
- Proposed duration and frequency of services to be provided.
- Estimated duration of episode of care.
An episode of outpatient therapy is defined as the period of time from the first day the member is under the care of the clinician for the current condition(s) being treated by one therapy discipline until the last date of service for that plan of care for that discipline in that setting.
Under state law, once every 90 days, the therapist's plan of care must be reviewed, revised if necessary, and signed as medically necessary by the member's physician or other licensed practitioner of the healing arts within the practitioner's scope of practice.
The care plan may not cover more than a 90-day period or the time frame documented in the approved IFSP.
A plan of care must be certified. Certification is the physician's, physician's assistant or nurse practitioner's approval of the plan of care. Certification requires a dated signature on the plan of care or some other document that indicates approval of the plan of care. If the service is a Medicare-covered service and is provided to a member who is eligible for Medicare, the plan of care must be reviewed at the intervals required by Medicare.
Re-Evaluation
A re-evaluation must occur whenever there is an unanticipated change in the member's status, a failure to respond to interventions as expected, or there is a need for a new plan of care based on new problems and goals requiring significant modification of treatment plan. Re-evaluation documentation does not need to be as comprehensive as the initial evaluation, but it must include at least the following:
- Reason for re-evaluation.
- Member's health and functional status reflecting any changes.
- Findings from any repeated or new examination elements.
- Changes to plan of care.
Visit/Encounter Notes
Written documentation of each encounter must be in the member's record of service. These visit notes document the implementation of the plan of care established by the therapist at the initial evaluation. Each visit note must include the following:
- The member's name and date of birth.
- The date of service.
- The type of service provided to the member.
- Total timed code treatment minutes and total treatment time in minutes.
- Total treatment time includes the minutes for timed code treatment and untimed code treatment.
- Total treatment time does not include time for services that are not billable (e.g., rest periods).
- Total treatment time includes the time spent providing each service. The number of units billed/requested must match the documentation (billing and the total timed code treatment minutes must be consistent).
In addition to the above required information items, the visit note documentation must contain the Subjective, Objective, Assessment and Plan format elements. These may be documented in any order (i.e., SOAP, APSO, etc.)
- A subjective element which includes the reason for the visit, the member/caregiver's report of the member's current status relative to treatment goals, and any changes in member's status since the last visit.
- An objective element which includes the practitioner's findings, including abnormal and pertinent normal findings from any procedures or tests performed.
- An assessment component which includes the practitioner's assessment of the member's response to interventions provided, specific progress made toward treatment goals, and any factors affecting the intervention or progression of goals.
- A plan component that states the plan for the next visit(s).
Discharge Summary
At the conclusion of therapy services, a discharge summary must be included in the documentation of the final visit in an episode of care. This must include the following:
- Highlights of a member's progress or lack of progress towards treatment goals.
- Summary of the outcome of services provided during the episode of care.
Covered Services
Physical and Occupational Therapy services are covered if they are medically necessary as defined in 10 CCR 2505-10 Section 8.076.1.8 and meet the following criteria:
- Treatment services must be ordered by an eligible prescribing provider (Physician, Physician Assistant, or Advanced Practice Nurse) and be started within 28 days of the date ordered.
- Therapy services must be provided under a written treatment plan stating with specificity the member's condition, functional level, treatment objectives, the physicians order, plans for continuing care, modifications to the plan and the plans for discharge from treatment.
- In a manner consistent with accepted standards of medical practice, the service is found to be equally effective for a diagnosis or treatment compared to other less conservative or more costly treatment options.
- The service has a base of evidence (including peer-reviewed literature and/or clinical experience and judgment) to support the clinical reasoning and selection of interventions.
- The service is consistent with the member's confirmed diagnosis, and not in excess of the member's needs.
Non-Covered Services
- A member may receive outpatient physical therapy and occupational therapy services during the same period and service dates, however, duplicate therapy (the same therapy performed by both an OT and PT) may not be performed on the same dates of service. Duplicated services (in general, and those overlapped between PTs and OTs) are not covered.
- Art and craft activities for the purposes of recreation are not covered.
- Services that are experimental, investigational or provided as part of a clinical trial and have been determined not to be medically necessary are not covered.
- Supplies or pre-fabricated supplies that can be obtained from a medical supplier are not covered.
- Services for conditions of chronic pain that do not interfere with the member's functional status and that can be treated by routine nursing measures are not covered.
- Services not documented in the member's health care record are not covered.
- Services not part of the member's plan of care are not covered.
- Services specified in a plan of care that is not reviewed and revised as medically necessary by the member's physician (M.D. or D.O.), physician's assistant, nurse practitioner, or specified in an approved Individualized Family Service Plan (IFSP) for Early Intervention PT/OT are not covered.
- A therapeutic service that is denied Medicare payment because of the provider's failure to comply with Medicare requirements is not covered.
- Vocational or educational services, except as provided under IEP-related or waiver services are not covered.
- Psychosocial services are not covered.
- Educational, personal need and comfort therapies are not covered.
- Record keeping documentation and travel time (the transport and waiting time of a member to and from therapy sessions) is not reimbursable.
- Time spent for preparation, report writing, processing of claims or documentation regarding billing or service provision is not reimbursable.
Rehabilitative and Habilitative Therapy Definitions
Health First Colorado covers both rehabilitative and habilitative therapies for all age groups in accordance with the Affordable Care Act Essential Health Benefit provisions.
The Colorado Division of Insurance defined Habilitative services to be:
Services that help a person retain, learn, or improve skills and functioning for daily living that are offered in parity with, and in addition to, any rehabilitative services offered in Colorado's Essential Health Benefits benchmark plan. Parity in this context means of like type and substantially equivalent in scope, amount and duration.
Rehabilitative therapies are those meant to assist a member with recovery from an acute injury, illness or surgical recovery. Habilitative therapies are those meant to help the member retain, learn or improve skills and functions for daily living. This includes the treatment of long-term chronic conditions and meeting developmental milestones.
Additional Notes
- Habilitative therapies are not categorized as an Inpatient or Home Health benefit. 'Acute' and 'Long-term' therapies remain benefits per Home Health coverage.
- Habilitative therapies are not a benefit if provided in nursing facilities; Rehabilitative PT/OT remain benefits in that setting.
- Habilitative therapies should not be confused with Habilitation services found within Home and Community Based Services (HCBS) waivers.
Assistive Technology Assessments
The following billing policies are effective for Current Procedural Terminology (CPT) code 97755 to accommodate HB14- 1211. HB14-1211 requires that all Health First Colorado members seeking complex rehabilitation technology must have an initial Assistive Technology Assessment (complex rehabilitative technology evaluation/assessment) prior to receiving complex rehabilitation technology and follow-up assessments, as needed. Only licensed speech, physical, and occupational therapists may render this specialty evaluation. All providers using procedure code 97755 must follow these guidelines. The Department recognizes that only a portion of Assistive Technology Assessments will be used for complex rehabilitation technology evaluation/assessment. Providers will be asked upon PAR submission if the service is for a complex rehabilitation technology assessment.
Policy Notes Complex rehabilitation technology evaluations / assessments are billed using only code 97755. Combinations of procedure codes, including procedure code 97542, for the purposes of complex rehabilitation technology evaluation / assessment are not allowed. Code 97755 always requires PAR. PARs must be submitted electronically using ColoradoPAR. Visit the ColoradoPAR web page for details. Member daily limit of code 97755 is 20 units. Up to five hours of assessment is allowed per date of service. Member yearly limit of code 97755 is 60 units. Members may have up to 60 units of procedure code 97755 per State Fiscal Year (July 1 - June 30). This limit will reset with the start of each new State Fiscal Year. PARs for procedure code 97755 must comply with the following policies:
- Must have a current prescription/referral for an Assistive Technology Assessment from the member's primary care physician.
- May indicate up to one (1) year duration.
- May indicate initial/new assessments or follow-up assessment visits.
- Only one (1) active PAR for code 97755 is allowed per member, per span of time. Overlapping code 97755 PAR requests will be denied.
- Initial PT/OT evaluation services, such as procedure code 97161, are not required prior to requesting code 97755.
- Procedure code 97755 is separate from PT/OT and is not part of the PT/OT benefit limitation.
- PARs for code 97755 should be submitted independently from other services. The Medical PAR type should be selected for code 97755.
If a member requires further assessment by a different provider not indicated on the original PAR and that PAR is still active, then it must be closed by the original requesting provider. Once closed, a new PAR can be submitted. Members may request a 'change of provider' on their PAR by contacting the vendor directly. Refer to the Prior Authorization Request (PARs) section of this manual.
Benefit Limitations
- A daily limit of five units of physical therapy services and five units of occupational therapy services is allowed, whether it is rehabilitative or habilitative. Some specific daily limits per procedure code apply.
- Providers are required to consult the American Medical Association's (AMA) Current Procedural Terminology (CPT) manual for each coded service. Some codes represent a treatment session without regard to its length of time (one unit maximum) while other codes may be billed incrementally as "timed" units.
Co-Treatment Policy
Co-treatment sessions between two outpatient therapists (pediatric behavioral therapists, physical therapists, occupational therapists and/or speech-language pathologists) are a covered service under the following conditions:
- Valid clinical rationale for providing co-treatment must be present. Providers should refer to the Joint Guidelines for Therapy Co-Treatment developed by the American Speech-Language-Hearing Association (ASHA), American Occupational Therapy Association (AOTA), and American Physical Therapy Association (APTA).
- Each provider must have an approved Plan of Care (or IFSP for Early Intervention) which includes co-treatment.
- Each provider must have an approved Prior Authorization which includes the Plan of Care/IFSP documentation that co-treatment will be used.
- Each provider may only bill for the time they directly treat the member during the co-treatment session. Direct treatment means a one-on-one treatment interaction between the provider and the member and does not include observation. The intent of the Department is to not reimburse twice for the same increments of time the member receives treatment. Direct treatment times are not required to be contiguous spans of time and may be broken-up as the therapists alternate interacting with the member. The providers must then only bill for the total amount of time they individually spent providing direct treatment.
Co-Treatment Reporting Example
A child receives one (1) hour of co-treatment involving a Pediatric Behavioral Therapist and a Speech Therapist. While both providers are with the child for the full hour, during that time the Speech Therapist provides direct treatment for 30 minutes and the Pediatric Behavioral Therapist provides direct treatment for 30 minutes.
The Speech Therapist would report one (1) unit of Current Procedural Terminology (CPT) 92507, because CPT 92507 is a visit-based unit regardless of time. The Pediatric Behavioral Therapist would report two (2) units of CPT 97153, because CPT 97153 is billed in increments of 15 minutes.
National Correct Coding Initiative (NCCI)
National Correct Coding Initiative Procedure-To-Procedure (PTP) and Medically Unlikely Edits (MUE) apply to certain combinations of PT and OT procedure codes. Visit the Centers for Medicare & Medicaid Services (CMS) NCCI web page for a complete list of impacted codes, guidance on bypass modifier uses and general information.
Coding Tables
Allowed Places of Service Codes
The following place of service codes are allowed:
Place of Service (POS) code Description 02 Telemedicine - Not provided in patient’s home (only applicable to certain procedure codes). Refer to the Telemedicine Billing Manual. 03 School 10 Telehealth - Provided in patient’s home. Refer to the Telemedicine Billing Manual. 11 Office 12 Home 13 Assisted Living Facility 62 Comprehensive Outpatient Rehabilitation Facility 99 Other - community location Effective May 3, 2024, place of service 03 is an allowed place of service for all fee-for-service benefits. In order for community providers to bill fee-for-service to children in a school setting, the provider must follow school district policy. Please reference the Community Providers in a School Setting Policy Memo.
- Telemedicine place of service (POS) code 02 is available for specific procedure codes. Visit the Telemedicine - Provider Information web page for a list of allowed procedure codes.
- Therapy services provided at an Outpatient Hospital are reported on the institutional claim type and are reimbursed as part of the hospital's EAPG payment. Institutional claim types do not have the POS code field.
- Therapy services provided at a Federally Qualified Health Center (FQHC) and Rural Health Clinic (RHC) are billed as part of the encounter rate for the center. They must not be billed separately on professional claims.
- POS code '99' is used for community locations (such as a library or grocery store) where services took place which are not better described as 'home', which is for the member's place of residence.
- Early Intervention providers may report any POS code which aligns with the treatment ordered by the child's Individualized Family Service Plan.
Outpatient Therapy Type Modifier 1 Modifier 2 Rehabilitative Physical Therapy GP 97 Rehabilitative Occupational Therapy GO 97 Habilitative Physical Therapy GP 96 Habilitative Occupational Therapy GO 96 Early Intervention Physical Therapy GP TL Early Intervention Occupational Therapy GO TL Allowed Outpatient PT/OT Procedure Codes
Physical and Occupational Therapists are indicated as rendering providers for the following procedures. Refer to the current Fee Schedule for rates. Evaluation and orthotic services are not subject to the 48-unit limit.
This table serves only as a reference guide and not a guarantee of payment or coverage. Definitive coverage of a specific procedure code is found on the Fee Schedule.
- Report procedure codes 97001, 97002, 97003, 97004 for evaluation services performed prior to 12/31/2016. Report procedure codes 97161-97168 for evaluation services performed on/after 1/1/2017.
- NCCI MUEs stipulate maximum daily units for each code. Visit the NCCI web page for further information.
- Providers should reference official AMA CPT resources for full descriptions of codes and instruction for proper use.
Table Updated: July 2024
Procedure Code Provider Type Prior Authorization Required Comments 92526 OT Does not require a PAR for the first 48 units; requires a PAR after 48 units are utilized. 90911 PT, OT No Ended 12-31-2019 90912 PT, OT No Effective 1-1-2020 90913 PT, OT No Effective 1-1-2020 96112 PT, OT No Effective 1-1-2020 96113 PT, OT No Effective 1-1-2020 97010 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97012 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97014 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97016 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97018 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97022 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97024 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97026 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97028 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97032 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97033 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97034 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97035 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97036 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97110 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97112 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97113 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97116 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97124 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97127 - - Not Covered. Refer to G0515. 97129 PT, OT Always Effective 1/1/2020 97130 PT, OT Always Effective 1/1/2020 97140 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97150 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97161 PT No 97162 PT No 97163 PT No 97164 PT No 97165 OT No 97166 OT No 97167 OT No 97168 OT No 97530 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. G0515 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. Closed 12/31/2019 97533 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97535 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97537 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97542 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97545 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97546 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97597 PT, OT No 97598 PT, OT No 97602 PT, OT No 97750 PT, OT No 97755 PT, OT Always Modifiers 96 or 97 are not required for this procedure code as this evaluation cannot be classified as either 'rehabilitative' or 'habilitative'. 97760 PT, OT No 97761 PT, OT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. 97763 PT, OT No 20560 PT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. Effective 1/1/2020 20561 PT Does not require a PAR for the first 48 units; requires PAR after 48 units are utilized. Effective 1/1/2020 L1902 PT, OT No L1960 PT, OT No L3730 PT, OT No L3763 PT, OT No L3764 PT, OT No L3808 PT, OT No L3900 PT, OT No L3906 PT, OT No L3908 PT, OT No L3912 PT, OT No L3919 PT, OT No L3923 PT, OT No L3925 PT, OT No L3929 PT, OT No L3933 PT, OT No L3982 PT, OT No Q4040 PT, OT No Q4048 PT, OT No Refer to the Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) Billing Manual located on the Billing Manuals web page under the CMS 1500 (Professional) drop-down section for further billing information on the above orthotic/prosthetic codes.
Reporting of Service Units
A. Timed and Untimed Codes
When reporting service units for CPT/HCPCS codes where the procedure is not defined by a specific timeframe ("untimed" CPT/HCPCS), the provider enters "1" in the field labeled "units." For untimed codes, units are reported based on the number of times the procedure is performed, as described in the CPT/HCPCS code definition.
Example: A member received a speech-language pathology evaluation represented by HCPCS "untimed" code 92521. Regardless of the number of minutes spent providing this service, only one unit of service is appropriately billed on the same day.
Several CPT codes used for therapy modalities, procedures, tests and measurements specify that the direct (one-on-one) time spent in patient contact is 15 minutes. Providers report these "timed" procedure codes for services delivered on any single calendar day using CPT codes and the appropriate number of 15-minute units of service.
Example: A member received a total of 60 minutes of occupational therapy, e.g., HCPCS "timed" code 97530 which is defined in 15-minute units, on a given date of service. The provider would then report 4 units of code 97530.
B. Counting Minutes for Timed Codes in 15-Minute Units
When only one service is provided in a day, providers should not bill for services performed for less than 8 minutes. For any single timed CPT code in the same day measured in 15-minute units, providers bill a single 15-minute unit for treatment greater than or equal to 8 minutes through and including 22 minutes. If the duration of a single modality or procedure in a day is greater than or equal to 23 minutes, through and including 37 minutes, then 2 units should be billed. Time intervals for 1 through 8 units are as follows:
Units Number of Minutes
1 unit: • 8 minutes through 22 minutes 2 units: • 23 minutes through 37 minutes 3 units: • 38 minutes through 52 minutes 4 units: • 53 minutes through 67 minutes 5 units: • 68 minutes through 82 minutes 6 units: • 83 minutes through 97 minutes 7 units: • 98 minutes through 112 minutes 8 units: • 113 minutes through 127 minutes The pattern remains the same for treatment times in excess of 2 hours.
When more than one service represented by 15-minute timed codes is performed in a single day, the total number of minutes of service (as noted on the chart above) determines the number of timed units billed. Refer to Example 1 below.
If any 15-minute timed service that is performed for 7 minutes or less than 7 minutes on the same day as another 15-minute timed service that was also performed for 7 minutes or less and the total time of the two is 8 minutes or greater than 8 minutes, then bill one unit for the service performed for the most minutes. This is correct because the total time is greater than the minimum time for one unit. The same logic is applied when three or more different services are provided for 7 minutes or less than 7 minutes. Refer to Example 5 below.
This Physical and Occupational Billing Manual and the Documentation Requirements section in the Speech Therapy Billing Manual indicates that the amount of time for each specific intervention/modality provided to the member is required to be documented in the Visits/Encounter Note. The total number of timed minutes must be documented. These examples indicate how to count the appropriate number of units for the total therapy minutes provided.
24 minutes of neuromuscular reeducation, code 97112,
23 minutes of therapeutic exercise, code 97110,
Total timed code treatment time was 47 minutes.Refer to the chart above. The 47 minutes falls within the range for 3 units = 38 to 52 minutes.
Appropriate billing for 47 minutes is only 3 timed units. Each of the codes is performed for more than 15 minutes, so each shall be billed for at least 1 unit. The correct coding is 2 units of code 97112 and one unit of code 97110, assigning more timed units to the service that took the most time.
20 minutes of neuromuscular reeducation (97112)
20 minutes therapeutic exercise (97110),
40 Total timed code minutes.Appropriate billing for 40 minutes is 3 units. Each service was done at least 15 minutes and should be billed for at least one unit, but the total allows 3 units. Since the time for each service is the same, choose either code for 2 units and bill the other for 1 unit. Do not bill 3 units for either one of the codes.
33 minutes of therapeutic exercise (97110),
7 minutes of manual therapy (97140),
40 Total timed minutesAppropriate billing for 40 minutes is for 3 units. Bill 2 units of 97110 and 1 unit of 97140. Count the first 30 minutes of 97110 as two full units. Compare the remaining time for 97110 (33-30 = 3 minutes) to the time spent on 97140 (7 minutes) and bill the larger, which is 97140.
18 minutes of therapeutic exercise (97110),
13 minutes of manual therapy (97140),
10 minutes of gait training (97116),
8 minutes of ultrasound (97035),
49 Total timed minutesAppropriate billing is for 3 units. Procedures would be billed based on the most provider time spent. Bill 1 unit each of 97110, 97116, and 97140. Ultrasound would not be billed because the total time of timed units that can be billed is constrained by the total timed code treatment minutes (i.e., providers may not bill 4 units for less than 53 minutes regardless of how many services were performed). Ultrasound would still be documented in the treatment notes.
7 minutes of neuromuscular reeducation (97112)
7 minutes therapeutic exercise (97110)
7 minutes manual therapy (97140)
21 Total timed minutesAppropriate billing is for one unit. The qualified professional shall select one appropriate CPT code (97112, 97110, 97140) to bill since each unit was performed for the same amount of time and only one unit is allowed.
Note: The above schedule of times is intended to provide assistance in rounding time into 15-minute increments. It does not imply that any minute until the eighth should be excluded from the total count. The total minutes of active treatment counted for all 15-minute timed codes includes all direct treatment time for the timed codes. Total treatment minutes, including minutes spent providing services represented by untimed codes, are also documented.
C. Determining What Time Counts Towards 15-Minute Timed Codes
Providers report the code for the time literally spent in the delivery of the modality requiring constant attendance and therapy services. Pre- and post-delivery services are not to be counted in determining the treatment service time. In other words, the time counted as "intra-service care" begins when the therapist or physician (or an assistant under the supervision of a physician or therapist) is directly working with the patient to deliver treatment services. The patient should already be in the treatment area (e.g., on the treatment table or mat or in the gym) and prepared to begin treatment.
The time counted is the time the patient is treated. For example, if gait training for a patient with a recent stroke requires both a therapist and an assistant or even two therapists to support during the use of the parallel bars, each 15 minutes the patient is being treated can count as only one (1) unit of code 97116. The time the patient spends not being treated during rests or bathroom breaks should not be billed. In addition, the time spent waiting to use a piece of equipment or for other treatment to begin is also not considered treatment time.
Treatment time for untimed codes is not counted towards the total treatment time for 15-minute unit codes.
Prior Authorization Requests (PARs)
Providers must submit PARs for medically necessary services when services will exceed 48 units of service per 12-month period.
PARs are approved for up to a 12-month period depending on medical necessity determined by the reviewer.
- Retroactive PAR request forms will not be accepted.
- Overlapping PAR request dates for same provider types will not be accepted, with the exception of Early Intervention PAR requests which may have overlapping dates of service and multiple provider types. All Early Intervention PT/OT PARs must additionally indicate that the member has an Individual Family Service Plan (IFSP) and that it is current and approved.
- Only one PAR for Early Intervention outpatient PT/OT may be active at a time.
- A maximum of one PAR for Early Intervention outpatient PT/OT and one PAR for non-Early Intervention outpatient PT/OT may be active at any time for children ages 0 - 4.
- Overlapping Early Intervention and non-Early Intervention outpatient PT/OT PARs will only be accepted if the treatment plans associated with each meet different goals and use different treatments.
- Incomplete, incorrect or insufficient member information on a PAR request form will not be accepted.
- An approved Individualized Family Service Plan serves as medical necessity, an order/prescription, and a Plan of Care.
Submit PARs for the number of units for each specific procedure code requested, not for the number of services. Modifier codes must be included. The same modifiers used on the PAR must be used on the claim, in the same order.
- When submitting Rehabilitative Therapy PARs and subsequent claims, CPT codes for PT services must have the GP modifier and the 97 modifier (e.g., 97110+GP+97). CPT codes for OT services must have the GO modifier and 97 modifier (e.g., 97110+GO+97).
- When submitting Habilitative Therapy PARs and subsequent claims, CPT codes for PT services must have the GP modifier and 96 modifier (e.g., 97110+GP+96). CPT codes for OT services must have the GO modifier and 96 modifier (e.g., 97110+GO+96).
- Early Intervention PARs and subsequent claims must have the GP or GO modifier plus the TL modifier (e.g., 97110+GP+TL).
Additional Limitations
- Members may have one (1) active PAR for each type of therapy (Rehabilitative PT, Rehabilitative OT, Habilitative PT, and Habilitative OT) with independent time spans. These PARs may not overlap in time span unless one of them is for Early Intervention.
- Evaluation and orthotic services do not require a PAR.
PAR Requirements
- Legibly written and signed ordering practitioner prescription, approved Plan of Care or approved Individualized Family Service Plan should include:
- Diagnosis (preferably with ICD-10 code).
- Reason for therapy.
- The number of requested therapy sessions per week.
- Total duration of therapy.
The authorizing agency reviews all completed PARs and approves or denies, by individual line item, each requested service or supply listed on the PAR. PAR status inquiries can be made through the Provider Web Portal and results are included in PAR letters sent to both the provider and the member. Read the results carefully as some line items may be approved and others denied. Do not render or bill for services until the PAR has been processed.
The claim must contain the PAR number for reimbursement. If the PAR is denied, providers should direct inquiries to the authorizing agency located on the Provider Contacts web page.
Billing Information
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down section for general billing information.
Ordering, Prescribing and Referring Billing Mandate
Effective July 1, 2022, the Department of Health Care Policy & Financing (the Department) started soft enforcement of the federal requirement 42 CFR § 455.440 that claims for certain types of services contain the National Provider Identifier (NPI) of the provider who ordered the service, and that the NPI is actively enrolled with Health First Colorado.
Effective July 1, 2024, all Outpatient Physical and Occupational Providers are required to enter the NPI of the ordering provider into the following locations for claim submission. In the Provider Web Portal, this field may be labeled as "Referring Provider." If the OPR NPI is missing on the claim, the claim will deny. Refer to the Resources section at the bottom of the Physical and Occupational Therapy Ordering, Prescribing, and Referring (OPR) Stakeholder Engagement web page.
Professional Claims
- Paper claims use field 17.b.
- Electronic submissions use loop 2420 with qualifier DK (Ordering), DN (Referring), or DQ (Supervising).
Institutional Claims
- The Attending Provider field (#76) or the Other ID fields (#78 or #79) for both paper and electronic claims.
- Providers may refer to their applicable UB-04 billing manuals for guidance on how each field is used.
Contact the Provider Services Call Center for assistance with claim submission.
Billing Edits
The provider's adherence to the application of policies in this manual is monitored through either post-payment review of claims by the Department, computer audits or edits of claims. When computer audits or edits fail to function properly, the application of policies in this manual remain in effect. Therefore, all claims shall be subject to review by the Department.
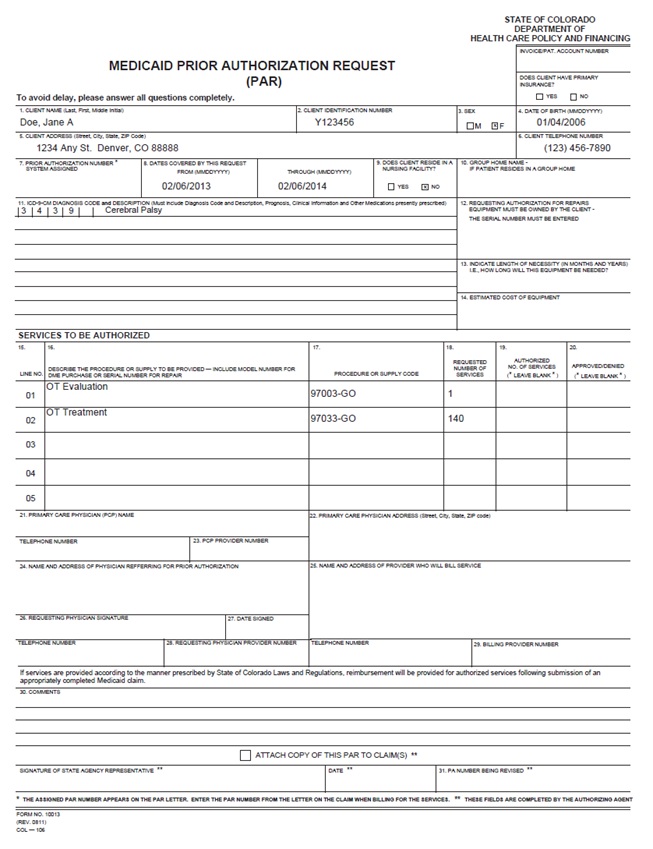
Occupational Therapy PAR Form Example
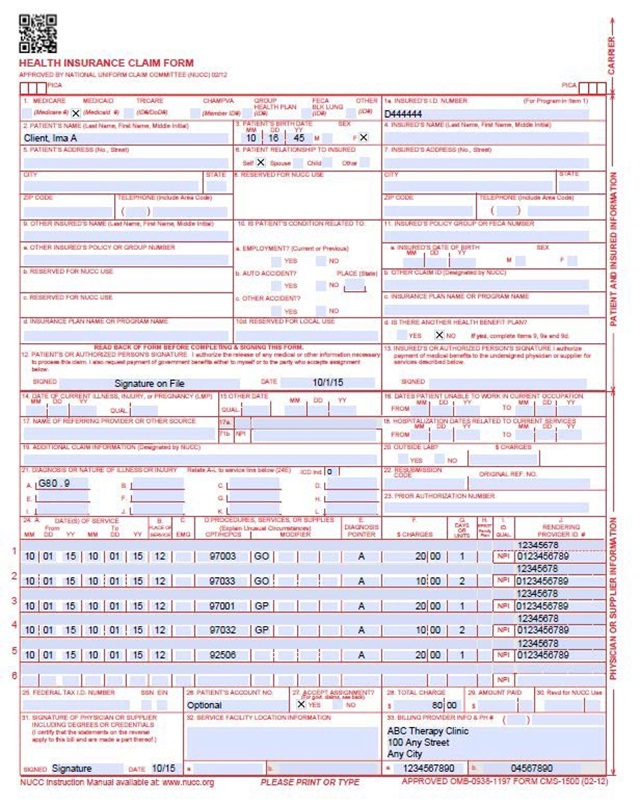
CMS 1500 Paper Claim Reference Table
The following paper form reference table shows required, optional and conditional fields and detailed field completion instructions for the CMS 1500 claim form.
CMS Field Number and Label Field Instructions 1. Insurance Type Required Place an "X" in the box marked as Medicaid. 1a. Insured's ID Number Required Enter the member's seven-digit Health First Colorado ID number as it appears on the Health First Colorado Identification card. Example: A123456. 2. Patient's Name Required Enter the member's last name, first name, and middle initial. 3. Patient's Date of Birth/Sex Required Enter the member's birth date using two digits for the month, two digits for the date, and two digits for the year. Example: 070124 for July 1, 2024. Enter the insured's birth date using two digits for the month, two digits for the date and two digits for the year. Example: 070124 for July 1, 2024.
The field accommodates the entry of two dates: a "From" date of services and a "To" date of service. Enter the date of service using two digits for the month, two digits for the date and two digits for the year. Example: 010124 for January 1, 2024.
From To 01 01 24 From To 01 01 24 01 01 24 Span dates of service
From To 01 01 24 01 31 24 Single Date of Service: Enter the six-digit date of service in the "From" field. Completion of the "To field is not required. Do not spread the date entry across the two fields.
Span billing: permissible if the same service (same procedure code) is provided on consecutive dates.
Supplemental Qualifier
To enter supplemental information, begin at 24A by entering the qualifier and then the information.
ZZ - Narrative description of unspecified code
VP - Vendor Product Number
OZ - Product Number
CTR - Contract Rate
JP - Universal/National Tooth Designation
JO - Dentistry Designation System for Tooth and Areas of Oral CavityEnter the Place of Service (POS) code that describes the location where services were rendered. Health First Colorado accepts the CMS place of service codes.
All procedures must be identified with codes in the current edition of Physicians Current Procedural Terminology (CPT). CPT is updated annually.
HCPCS Level II Codes
The current Medicare coding publication (for Medicare crossover claims only).Enter the appropriate procedure-related modifier that applies to the billed service. Up to four modifiers may be entered when using the paper claim form.
At least one diagnosis code reference letter must be entered.
When multiple services are performed, the primary reference letter for each service should be listed first, other applicable services should follow.
Some CPT procedure codes are grouped with other related CPT procedure codes. When more than one procedure from the same group is billed, special multiple pricing rules apply.
The base procedure is the procedure with the highest allowable amount. The base code is used to determine the allowable amounts for additional CPT surgical procedures when more than one procedure from the same grouping is performed.
Submitted charges cannot be more than charges made to non-Health First Colorado covered individuals for the same service.
Anesthesia Services
Anesthesia services must be reported as minutes. Units may only be reported for anesthesia services when the code description includes a time period.Anesthesia time begins when the anesthetist begins member preparation for induction in the operating room or an equivalent area and ends when the anesthetist is no longer in constant attendance. No additional benefit or additional units are added for emergency conditions or the member's physical status.
The fiscal agent converts reported anesthesia time into fifteen-minute units. Any fractional unit of service is rounded up to the next fifteen-minute increment.
Each claim must have the date the enrolled provider or registered authorized agent signed the claim form. Enter the date the claim was signed using two digits for the month, two digits for the date and two digits for the year. Example: 070124 for July 1, 2024.
CMS 1500 OT/PT Claim Example
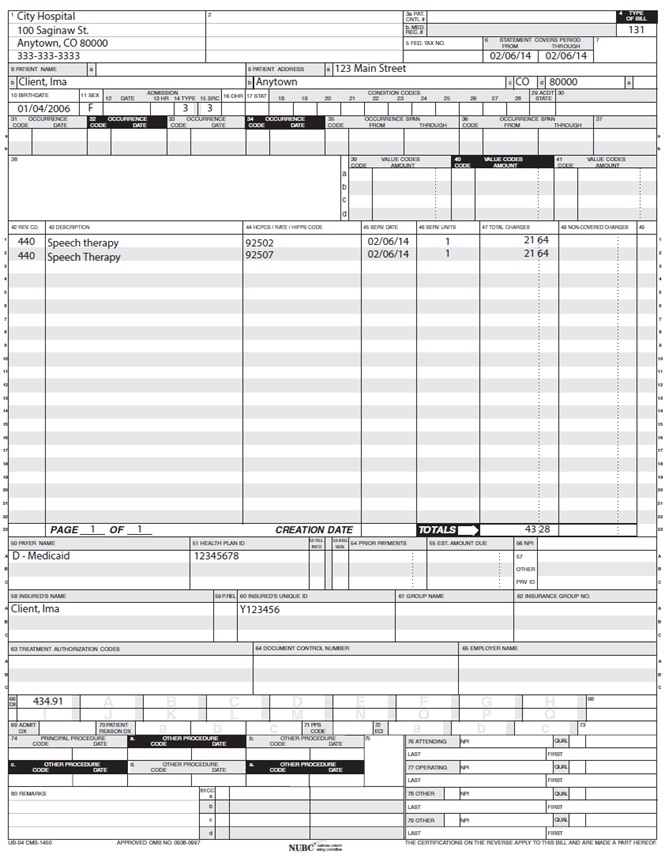
UB-04 Paper Claim Reference Table
PT and OT outpatient hospital paper claims must be submitted on the UB-04 claim form.
The information in the following Paper Claim Reference Table lists the required, optional and/or conditional form locators for submitting the UB-04 paper claim form to Health First Colorado for PT and OT services. It also provides instructions for completing Form Locators (FL) as they appear on the paper UB-04 claim form. Instructions for completing the UB-04 claim form are based on the current National Uniform Billing Committee (NUBC) UB-04 Reference Manual. Unless otherwise noted, all data FLs on the UB-04 have the same attributes (specifications) for Health First Colorado as those indicated in the NUBC UB-04 Reference Manual.
All code values listed in the NUBC UB-04 Reference Manual for each FL may not be used for submitting paper claims to Health First Colorado. The appropriate code values listed in this manual must be used when billing Health First Colorado.
Required
Enter the provider or agency name and complete mailing address of the provider who is billing for the services:Abbreviate the state using standard post office abbreviations. Enter the telephone number.
Required only if different from FL 1.
Enter the provider or agency name and complete mailing address of the provider who will receive payment for the services:- Street/Post Office box City
- State Zip Code
Required
For PRTF, use TOB 89X.
Enter the three-digit number indicating the specific type of bill. The three-digit code requires one digit each in the following sequences (Type of facility, Bill classification, and Frequency):Digit 1 Type of Facility 1 Hospital 2 Skilled Nursing 3 Home Health Services 4 Religious Non-Medical Health Care Institution 6 Intermediate Care 7 Clinic (Rural Health/FQHC/Dialysis Center) 8 Special Facility (Hospice, RTCs) Digit 2 Bill Classification (except clinics and special facilities): 1 Inpatient (Including Medicare Part A) 2 Inpatient (Medicare Part B only) 3 Outpatient 4 Other (for hospital referenced diagnostic services or home health not under a plan of treatment) 5 Intermediate Care Level I 6 Intermediate Care Level II 7 Sub-Acute Inpatient (Revenue Code 019X required with this bill type) 8 Swing Beds 9 Other Digit 2 Bill Classification (Clinics Only): 1 Rural Health/FQHC 2 Hospital Based or Independent Renal Dialysis Center 3 Freestanding 4 Outpatient Rehabilitation Facility (ORF) 5 Comprehensive Outpatient Rehabilitation Facilities (CORFs) 6 Community Mental Health Center Digit 2 Bill Classification (Special Facilities Only): 1 Hospice (Non-Hospital Based) 2 Hospice (Hospital Based) 3 Ambulatory Surgery Center 4 Freestanding Birthing Center 5 Critical Access Hospital 6 Residential Facility Digit 3 Frequency: 0 Non-Payment/Zero Claim 1 Admit through discharge claim 2 Interim - First claim 3 Interim - Continuous claim 4 Interim - Last claim 7 Replacement of prior claim 8 Void of prior claim Enter the From (beginning) date and Through (ending) date of service covered by this bill using MMDDYY format. Example: January 1, 2024 = 0101024
Member requires immediate intervention as a result of severe, life threatening or potentially disabling conditions.
Exempts inpatient hospital and clinic claims from co-payment and PCP referral.
Exempts outpatient hospital claims from co- payment and PCP only if revenue code 450 or 459 is present.
This is the only benefit service for an undocumented alien.
If span billing, emergency services cannot be included in the span bill and must be billed separately from other outpatient services.
1- Urgent
The member requires immediate attention for the care and treatment of a physical or mental disorder.2- Elective
The member's condition permits adequate time to schedule the availability of accommodations.3- Newborn
Required for inpatient and outpatient hospital.4- Trauma Center
Visit to a trauma center/hospital as licensed or designated by the state or local government authority authorized to do so, or as verified by the American College of Surgeons and involving trauma activation.Required
Enter the appropriate code for co-payment exceptions on claims submitted for outpatient services. (To be used in conjunction with FL 14, Type of Admission).1 Physician referral 2 Clinic referral 3 Referred from HMO 4 Transfer from a hospital 5 Transfer from a skilled nursing facility (SNF) 6 Transfer from another health care facility 7 Emergency Room 8 Court/Law Enforcement 9 Information not available A Transfer from a Critical Access Hospital B Transfer from another Home Health Agency C Readmission to Same Home Health Agency Newborns 1 Normal Delivery 2 Premature Delivery 3 Sick Baby 4 Extramural Birth (Birth in a non- sterile environment) 01 Discharged to Home or Self Care (Dialysis is limited to code 01) 02 Discharged/transferred to another short-term hospital 70 Discharged/Transferred to Other HC Institution 71 Discharged/transferred/referred to another institution for outpatient services 72 Discharged/transferred/referred to this institution for outpatient services Use code 02 for a PPS hospital transferring a patient to another PPS hospital. Code 05, Discharged to Another Type Institution, is the most appropriate code to use for a PPS hospital transferring a patient to an exempt hospital.
**A PPS hospital cannot use Patient Status codes 30, 31 or 32 on any claim submitted for DRG reimbursement. The code(s) are valid for use on exempt hospital claims only.
Interim bills may be submitted for Prospective Payment System (PPS)-DRG claims but must meet specific billing requirements.
For exempt hospitals use the appropriate code from the codes listed.
Note: Refer to the "Interim" billing instruction in this section of the manual.
Complete with as many codes necessary to identify conditions related to this bill.
Condition Codes
01 Military service related 02 Employment related 04 HMO enrollee 05 Lien has been filed 06 ESRD patient - First 18 months entitlement 07 Treatment of non-terminal condition/hospice patient 17 Patient is homeless 25 Patient is a non-US resident 39 Private room medically necessary 42 Outpatient Continued Care not related to Inpatient 44 Inpatient CHANGED TO Outpatient 51 Outpatient Non-diagnostic Service unrelated to Inpatient admit 60 DRG (Day outlier)Renal Dialysis Settings
71 Full care unit
72 Self-care unit
73 Self-care training
74 Home care
75 Home care - 100 percent reimbursement 76 Back-up facilitySpecial Program Indicator Codes
A1 EPSDT/CHAP
A2 Physically Handicapped Children's Program
A4 Family Planning
A6 PPV/Medicare
A9 Second Opinion Surgery
AA Abortion Due to Rape
AB Abortion Done Due to Incest
AD Abortion Due to Life Endangerment
AI Sterilization
B3 B4 Pregnancy IndicatorAdmission Unrelated to Discharge PRO Approval Codes
C1 Approved as billed
C2 Automatic approval as billed - Based on focused review
C3 Partial approval
C4 Admission/Services denied
C5 Post payment review applicable
C6 Admission preauthorization
C7 Extended authorizationConditional
Complete both the code and date of occurrence.
Enter the appropriate code and the date on which it occurred. Enter the date using MMDDYY format.
Occurrence Codes:1 Accident/Medical Coverage 2 Auto Accident - No Fault Liability 3 Accident/Tort Liability 4 Accident/Employment Related 5 Other Accident/No Medical Coverage or Liability Coverage 6 Crime Victim 20 Date Guarantee of Payment Began 24* Date Insurance Denied 25* Date Benefits Terminated by Primary Payer 26 Date Skilled Nursing Facility Bed Available 27 Date of Hospice Certification or Re- certification 40 Scheduled Date of Admission (RTD) 50 Medicare Pay Date 51 Medicare Denial Date 53 no longer used 55 Insurance Pay Date A3 Benefits Exhausted - Indicate the last date of service that benefits are available and after which payment can be made by payer A indicated in FL 50 B3 Benefits Exhausted - Indicate the last date of service that benefits are available and after which payment can be made by payer B indicated in FL 50 C3 Benefits Exhausted - Indicate the last date of service that benefits are available and after which payment can be made by payer C indicated in FL 50 *Other Payer occurrence codes 24 and 25 must be used when applicable. The claim must be submitted with the third-party information.
Conditional
Enter appropriate codes and related dollar amounts to identify monetary data or number of days using whole numbers, necessary for the processing of this claim. Never enter negative amounts. Codes must be in ascending order. If a value code is entered, a dollar amount or numeric value related to the code must always be entered.Most Common Codes:
01 semiprivate rate (Accommodation Rate) 06 Medicare blood deductible 14 No fault including auto/other 15 Worker's Compensation 31 Member Liability Amount* 32 Multiple Member Ambulance Transport 37 Pints of Blood Furnished 38 Blood Deductible Pints 40 New Coverage Not Implemented by HMO 45 Accident Hour
Enter the hour when the accident occurred that necessitated medical treatment. Use the same coding used in FL 18 (Admission Hour).49 Hematocrit Reading - EPO Related 58 Arterial Blood Gas (PO2/PA2) 68 EPO-Drug 80 Covered Days 81 Non-Covered Days Enter the deductible amount applied by indicated payer:
Deductible Payer A
B1 Deductible Payer B
C1 Deductible Payer CEnter the amount applied to member's co-insurance by indicated payer:
A2 Coinsurance Payer A
B2 Coinsurance Payer B
C2 Coinsurance Payer CEnter the amount paid by indicated payer:
A3 Estimated Responsibility Payer A
B3 Estimated Responsibility Payer B
C3 Estimated Responsibility Payer CFor Rancho Coma Score bill with appropriate diagnosis for head injury.
Medicare and TPL - Refer to A1-A3, B1-B3, and C1-C3 above.
Enter the revenue code which identifies the specific service provided. List revenue codes in ascending order. Valid dialysis revenue codes are listed in Appendix Q located on the Billing Manuals web page under the Appendices drop-down menu.
A revenue code must appear only once per date of service. * If more than one of the same service is provided on the same day, combine the units and charges on one line accordingly.
When billing outpatient hospital radiology, the radiology revenue code may be repeated, but the corresponding HCPCS code cannot be repeated for the same date of service. Refer to instructions under FL 44 (HCPCS/Rates).
Enter only the HCPCS code for each detail line. Use approved modifiers listed in this section for hospital-based transportation services.
Complete for laboratory, radiology, physical therapy, occupational therapy, and hospital-based transportation. When billing HCPCS codes, the appropriate revenue code must also be billed.
HCPCS codes must be identified for the following revenue codes:
- 030X Laboratory
- 032X Radiology - Diagnostic
- 033X Radiology - Therapeutic
- 034X Nuclear Medicine
- 035X CT Scan
- 040X Other Imaging Services
- 042X Physical Therapy
- 043X Occupational Therapy
- 054X Ambulance
- 061X MRI and MRA
HCPCS codes cannot be repeated for the same date of service. Combine the units in FL 46 (Units) to report multiple services.
The following revenue codes always require a HCPCS code.
When a HCPCS code is repeated more than once per day and billed on separate lines, use modifier 76 to indicate this is a repeat procedure and not a duplicate.
0252 Non-Generic Drugs 0253 Take Home Drugs 0255 Drugs Incident to Radiology 0257 Non-Prescription 0258 IV Solutions 0259 Other Pharmacy 0260 IV Therapy General Classification 0261 Infusion Pump 0262 IV Therapy/Pharmacy Services 0263 IV Therapy/Drug/Supply Delivery 0264 IV Therapy/Supplies 0269 Other IV Therapy 0631 Single Source Drug 0632 Multiple Source Drug 0633 Restrictive Prescription 0634 Erythropoietin (EPO) 0635 Erythropoietin (EPO) >,10,000 0636 Drugs Requiring Detailed Coding Each date of service must fall within the date span entered in the "Statement Covers Period" field (FL 6).
Enter incurred charges that are not payable by Health First Colorado.
Non-covered charges must be entered in both FL 47 (Total Charges) and FL 48 (Non-Covered Charges.) Each column requires a grand total on line 23.
Enter the payment source code followed by name of each payer organization from which the provider might expect payment.
At least one line must indicate Health First Colorado.Source Payment Codes B Workmen's Compensation C Medicare D Health First Colorado E Other Federal Program F Insurance Company G Blue Cross, including Federal Employee Program I Other Line A Primary Payer Line B Secondary Payer Line C Tertiary Payer Enter the procedure code for the principal procedure performed during this billing period and the date on which procedure was performed. Enter the date using MMDDYY format. Apply the following criteria to determine the principal procedure:
Complete when there are additional significant procedure codes.
If the attending physician is not enrolled in Health First Colorado or if the member leaves the ER before being seen by a physician, the hospital may enter their individual numbers.
Complete when attending physician is not the PCP or to identify additional physicians.
Ordering, Prescribing, or Referring NPI - when applicable
NPI - Enter up to two 10-digit NPI numbers, when applicable. This form locator identifies physicians other than the attending physician. If the attending physician is not the PCP or if a clinic is a PCP agent, enter the PCP NPI number as the referring physician. The name of the Health First Colorado member's PCP appears on the eligibility verification. Review either for eligibility or PCP. Health First Colorado does not require that the PCP number appear more than once on each claim submitted.
UB-04 Outpatient PT Claim Example
Timely Filing
Refer to the General Provider Information Manual located on the Billing Manuals web page under the General Provider Information drop-down section for more information on timely filing policy, including the resubmission rules for denied claims.
PT/OT Revisions Log
- Added telemedicine POS 02 reference to the Coding section.
- Added POS 13 to the Coding section (allowed retroactively to align with interChange configuration)
- Clarified that CPT 97755 does not require mod 96 or 97 in the coding table.
- Revised PAR requirement section to clarify that either a prescription or approved Plan of Care is necessary.